What prospects for mental health?
Since the start of the global pandemic in 2020, two words so far taboo have entered the collective language: mental health. By containing movements and interactions, the pandemic has affected the mental health of a large number of individuals.
Published on September 08th, 2022 at 10:06 am
It's one of the many contemporary factors which, according to the WHO, cause one in five people to suffer from mental disorders worldwide. A long-neglected ailment that can now be diagnosed and supported thanks to digital technology.
To understand what mental health is, the ecosystem of innovative companies that are already providing solutions, and the challenges ahead, we spoke to Dr. Fanny Jacq, psychiatrist, director of mental health at Qare, member of Future4care, and president of the MentalTech collective. Here, she shares her vision and some food for thought.
Psychiatry has long been the poor relation of medical innovation
Mental health, as defined by the World Health Organization (WHO), is "a state of complete physical, mental and social well-being... in which a person can realize his or her full potential, cope with the normal stresses of life, perform productively and contribute to the life of his or her community". This broad, positive definition makes it clear that mental health is not just the absence of mental disorders or illness, but an essential element of an individual's overall health. In other words, there can be no health without mental health.
Until now, however, mental health has mainly been associated with psychiatric disorders and pathologies, which include schizophrenia and other acute or chronic psychotic disorders, bipolar disorders, post-traumatic stress disorders, eating disorders, anxiety disorders, phobias, depression, burn-out, addictions (to screens, tobacco, alcohol, drugs), OCD, autistic disorders, but also personality disorders that can evolve into pathologies (borderline personality, for example). The manifestation of these disorders gives rise to highly heterogeneous clinical situations, with more or less incapacitating or chronic conditions depending on the individual.
These so-called mental illnesses have long been (and still are) stigmatized. In the early 19th century, "asylums", as they were called, were built outside towns. They had orchards, vegetable gardens, animals... so as to be self-sufficient and allow city-dwellers to avoid crossing paths with the sick.
Today, asylums have been renamed "specialized hospital centers" (CHS), but specialized in what? We're not told, and the word CHS is still taboo in psychiatry.
What's more, psychiatry has long been the poor relation when it comes to medical innovation. In fact, psychiatric care has remained much the same for the past 70 years. For the most part, it consists of an interview to ascertain symptoms, the completion of questionnaires by the patient, a diagnosis by the practitioner and the initiation of treatment: medication and/or psychotherapy.
But with appointments spaced several weeks apart (in the best of cases), and without knowing anything about the patient's life or environment outside the office consultations, it is very difficult to develop continuous, personalized follow-up.
This is why digital technologies, such as real-time patient data collection, have the potential to revolutionize the way we support, prevent and destigmatize mental illness.
Especially since mental health is a spectrum, not a binary phenomenon. People with mental disorders can enjoy good mental health. And conversely, it is possible to have poor mental health without suffering from mental illness. This is why we often speak of mental health as a continuum, likely to vary over the course of a lifetime through the action of a number of socio-economic, biological and environmental determinants.
We are facing one of the major economic and societal challenges of the century.
Mental health pathologies are the most costly area of expenditure for the French health insurance system (Assurance Maladie). Every year, it devotes over 23 billion euros to them, more than the resources allocated to cancer (18 billion euros) and cardiovascular diseases (13.4 billion euros).
Yet a study carried out a few months ago by the Institut Sapiens for the MentalTech collective showed that the development of digital innovations in the field of mental health would enable a reduction in logistical costs (transport, hospitalization) and consultation costs, as well as an increase in the number of patients monitored, an improvement in follow-up, care and compliance, and a reduction in the use of psychotropic drugs. The combination of these effects could lead to a sharp drop in expenditure, generating 5.9 billion euros a year in direct savings and 9.4 billion euros a year in indirect savings - a total gain of 15.3 billion euros. Not to mention the improved mental well-being of patients, earlier detection of disorders, and more personalized, rapid and effective management of disorders that could be achieved through the introduction of e-mental health technologies.
However, we had to wait until the second half of the 2010s to see the emergence of digital innovation in mental health, in the image of mobile applications Petit BamBou (2014), Kwit (2017) or Mon Sherpa (2019). This slowness can be explained by a structural phenomenon, linked to the healthcare sector itself, marked by regulatory, legal, approval, accreditation and data security constraints. As a result, the healthcare sector is generally the last to innovate, and mental health even more so, due to the obstacles and taboos mentioned above.
In the end, it's to the sanitary crisis that "we owe" the increase in the use of various mental e-health tools. While the Covid-19 pandemic has severely damaged the mental health of individuals around the world, it has also created new uses for patients. The latter have taken greater advantage of the tools offered by digital technology, starting with teleconsultation. The result: by 2021, more than 120 e-mental health startups had been created worldwide, and venture capitalists had poured a record $5.5 billion into mental health and wellness specialists, a 139% jump on the $2.3 billion in 2020.
Now that e-mental health solutions are becoming increasingly numerous, several classifications are possible.
By level of technology: easy-to-access solutions that can be easily reproduced and disseminated among users sit alongside "hard tech" technological solutions, which are more complex and require greater investment and engineering.
By type of audience: while some solutions are aimed at mental health professionals and others at caregivers, the vast majority are aimed at patients, who can themselves be divided into sub-categories: children and adolescents, adults, seniors - for example.
But the most relevant classification remains the placement of solutions on the care pathway, from prevention to curation. Upstream of the care pathway are primary, secondary and tertiary prevention solutions, as well as mental well-being and behavioral health solutions. Continuing along the pathway towards more curative functions, solutions provide diagnostic assistance, put patients in touch with a professional... right through to devices for treating identified pathologies.
The business models of these mental health startups also differ. We can already identify 5 ways of financing ourselves when addressing a mental health issue.
Non-medical wellness solutions such as Petit BamBou are self-financed and/or financed by private funds, and often operate on a "freemium" model: part of the functionality is available free of charge, and the complete solution is offered as a paid subscription (although other sources of revenue are possible, such as advertising revenue or database monetization).
Other solutions, such as Mon Sherpa, a chatbot for people in mental distress, are free. In this case, the free solution sometimes acts as a "call product" for services that may have to be paid for, such as chat with a therapist or teleconsultation with a healthcare professional.
Corporate mental health solutions such as mindDay, Lumm, Holivia or moka.care are based on a BtoB model. The final payer is the company offering these services to its employees.
Medical solutions for patients, such as HypnoVR or ResilEyes Therapeutics, fall within the scope of regulations governing digital medical devices. They must prove their clinical efficacy (and hence service rendered) to obtain CE marking, and submit a file to the Cnedimts to apply for reimbursement, the evaluation focusing on two aspects: health (in the clinical sense) and medico-economic contribution. For the moment, no digital medical device for mental health in France seems to have passed these two stages, but steps are underway and it's only a matter of time. The market for digital therapies is booming, and the news that a digital mental health plan is to be prepared for the autumn is very positive.
Another model that is developing rapidly is that of partnerships with mutual insurers or health insurance companies. In this case, the mutual company offers its members a healthcare solution in addition to the usual services. By broadening and diversifying its range of services, it develops an innovative approach that sets it apart from the competition.
The issue of well-being in the workplace is becoming inescapable
If more and more solutions are aimed directly at companies, it's because the cost to them of unhappiness at work is very high, in the region of €13,340 per employee per year, mainly due to absenteeism and the associated drop in productivity.
A third of the French people are affected by stress at work. A survey of general practitioners showed that when, they are consulted for reasons of anxiety or stress, work is the main cause.
New work organizations and the age of constant connection are generating new psycho-social risks. The constant state of alert in which working people find themselves weighs heavily on their mental health. The boundary between professional and personal life is no longer as clear-cut as it used to be ("blurring"), and not everyone has the resources to cope.
Questions of well-being at work or quality of working life (QWL) emerged in France in the 2000s. But here again, it seems it was the sanitary crisis that got the ball rolling: the term "mental health" has recently entered the corporate lexicon.
A PSYCHODON & OPINIONWAY survey restituted in April 2021 indicates that 76% of employees believe that the company is responsible for the mental health of its employees, but that only 31% of companies put in place resources to promote well-being.
The range of solutions available to companies wishing to take an interest in the mental well-being of their employees is vast, from simple awareness-raising actions to telemedicine solutions paid for by the employer - bearing in mind that they can be combined to multiply their effects.
As there are still many taboos and prejudices surrounding mental health, information and training are useful in deconstructing and changing representations. Numerous organizations, both private and associative, offer webinars, workshops and other awareness-raising conferences in the workplace. To take a step further, PSSM France offers a two-day course in Mental Health First Aid to train mental health first-aiders.
Self-help solutions provide first-level help, accessible 24/7: via a website, mobile app or chatbot, for example. The most sophisticated of these tools are based on the principles of cognitive psychology or behavioral health, and enable users to find support for mild symptoms, or as a complement to therapy. Examples include Alan Mind or Mon Sherpa, Qare's psychological support solution.
Solutions that put users in touch with psychologists, coaches and other therapists have multiplied since the sanitary crisis. If the decision to consult a therapist is a personal one, the company can nevertheless facilitate the process by removing any obstacles, particularly economic ones, to accessing care.
Finally, when it comes to consulting a psychiatrist, only telemedicine companies are authorized to offer teleconsultation. Qare, for example, offers companies a comprehensive health program combining prevention, 24/7 access to care in some fifty medical specialties, and medical follow-up.
It should be noted that all these steps require a more or less committed personal approach on the part of the employee, who will learn to take care of himself and ask for help if necessary. This is not to minimize the role played by the company as a whole. For it is up to the company to put in place a healthy, efficient work organization that enables a fair balance between professional and personal life.
If the players involved sometimes each one offload the burden onto the other, it's because the lack of well-being expressed at work is multifactorial. In the cases of burnouts, for example, it is generally accepted that 60% of the causes are organizational (i.e. attributable to the company), and 40% personal. While progress has been slow, it must be admitted that undeniable progress has been made on the employer's side. There is a growing awareness that emergency numbers are no longer enough, and that upstream action is needed to educate and prevent. Some companies are taking up the subject with great sincerity and commitment as part of their CSR approach, while others have only a reactive and short-sighted vision akin to "mental washing".
It is time to accelerate the development of this ecosystem
A first step has been taken, words have been spoken, actions have been taken, such as the Assises de la santé mentale organized for 2021. And this deserves to be emphasized. But it's still not enough. According to the WHO, depression will be the number one disease in the world by 2030, and mental illnesses are the most costly for Social Security. The measures and budgets allocated are not yet up to the task.
When it comes to financing companies that innovate for our mental health, the majority of deals (68%) in 2021 were with startups in the seed phase, demonstrating the market's lack of maturity.
In France, with the exception of Alan (€183 million), fund-raising by players operating in the field of mental health remains modest, as in the case of moka.care (€15 million) and HypnoVR (€4.5 million). Yet the financial survival of start-ups depends on it. For those embarking on the path to medical device status, and a fortiori reimbursability, it can take several years to get to market - years during which they will have to undertake costly clinical investigations, certification and medico-economic studies.
Although the French e-health ecosystem is highly dynamic, with over sixty players listed, it remains ultra-specialized, fragmented, immature and therefore potentially fragile. As shown in a study by the Institut Sapiens entitled "Construire l'Europe de la e-santé - Faire émerger des champions européens de la santé pour résister aux Big Tech étrangères" published in February 2022, the main challenge facing the e-health market lies in achieving a certain critical size. Regulatory facilitation is the key. Without it, there can be no European health data policy, no common development policy, and no innovation incubation structures. And yet, this favorable breeding ground is essential for the emergence and development of start-ups, enabling them to reach the necessary maturity.
If things aren't moving fast enough, the younger generations are very mobilized. They are hearing more and more about the importance of a good mind/body balance and the notion of mental health. In fact, the subject has become less taboo, and the word is getting out - thanks in particular to the stimulus of social networking accounts, artists like Stromae, and athletes like Simone Biles and Naomi Osaka. Everyone now dares to talk about mental health in an uninhibited, unfiltered way. Ideally, the subject should be brought up at school, from childhood onwards. Just as we teach sex education or civics, it's important to teach our children - tomorrow's adults - that there's no shame in expressing our emotions, our fears, our fragilities, and in asking for help if necessary. It's okay not to be okay!
Are you a mental health startup at an intermediate stage of development? Write to usto accelerate your time to market.
Thanks again to Dr. Fanny Jacq for her valuable advice.
----------------------
About the MentalTech collective
The MentalTech collective is the first French collective dedicated to the emergence and development of digital solutions in mental health. It was created in March 2022 by 7 founding members: hypnoVR, Kwit, mindDay, PetitBamBou, Qare, ResilEyes Therapeutics, and Tricky.
Its aim is to bring together private and public organizations around a single ambition: to respond to the urgent need to deploy ethical digital tools in the prevention and management of mental health, alongside healthcare professionals.
You may also like
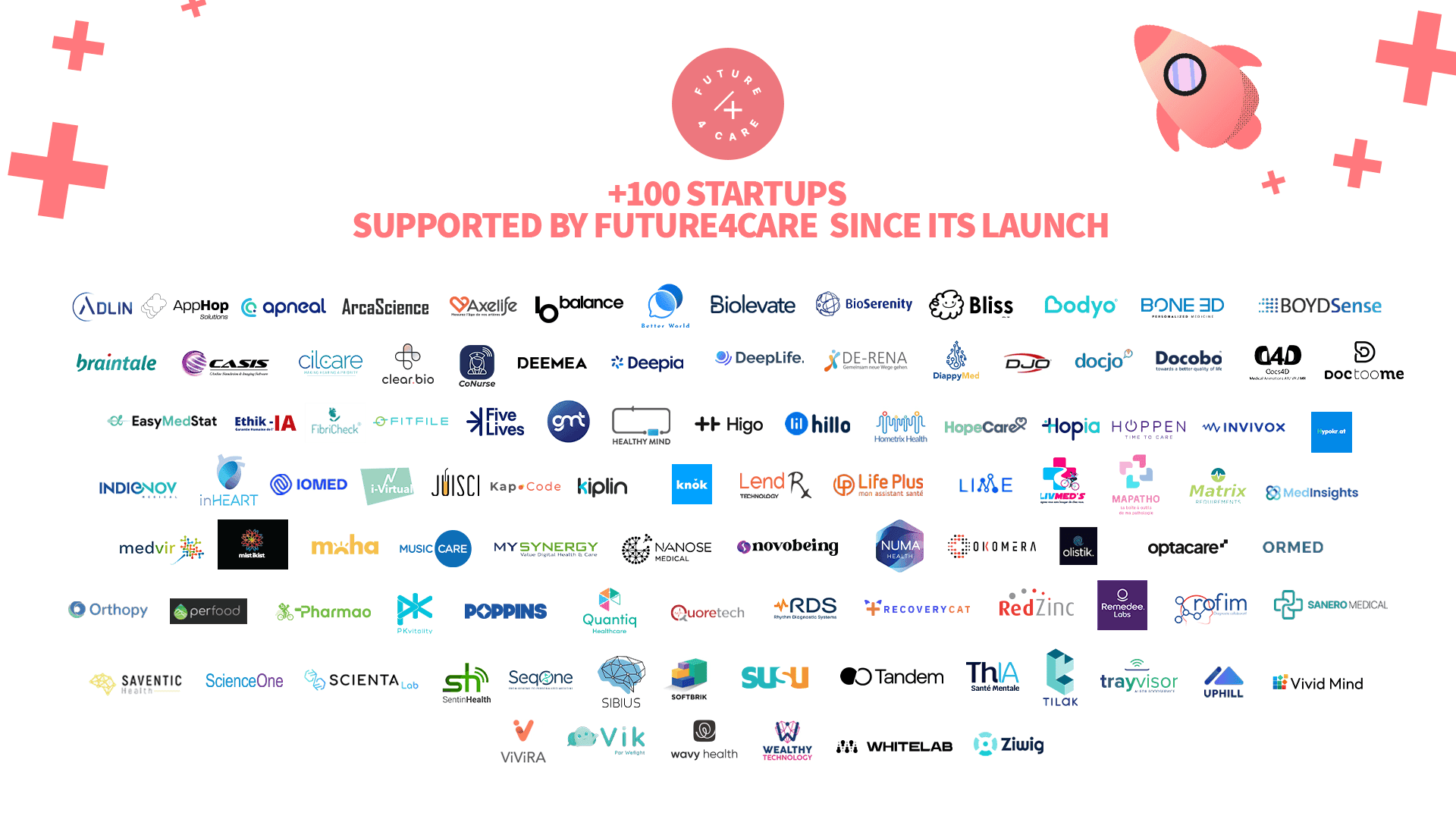
This year, Future4care celebrates a milestone: 100 startups supported on their journey to shaping the future of health.
Highlights from the Health Insurance and Social Protection Masterclass by TNP Consultants"
